Things to Know About MicroTESE Surgery
Microsurgical Testicular Sperm Extraction is a surgical treatment for retrieving sperm from a male testis. It is regarded as one of the most successful procedures of sperm retrieval and is used mostly in cases of severe infertility such as azoospermia (inability to make sperm).
MicroTESE is often used for men with non-obstructive azoospermia (NOA) where sperm production is low or absent. The need for prior procedures like needle aspiration or biopsy before MicroTESE is a subject of some debate. Some studies suggest these procedures may not be necessary, while others recommend them to assess sperm availability and guide the MicroTESE approach.
The microTESE success rate is fairly high. In fact, doctors can detect sperm approximately 60% of the time during microTESE procedures.
Many studies have also found that microTESE treatments produce the best rate of sperm retrieval while causing the least amount of harm to the testicles.
ICSI with Micro testicular sperm extraction (MicroTESE) can resolve many cases of sperm in the ejaculate and severe male factor infertility, assisting many couples in conception.
How Is MicroTESE Procedure Performed?
The following points explain the microTESE procedure in detail:
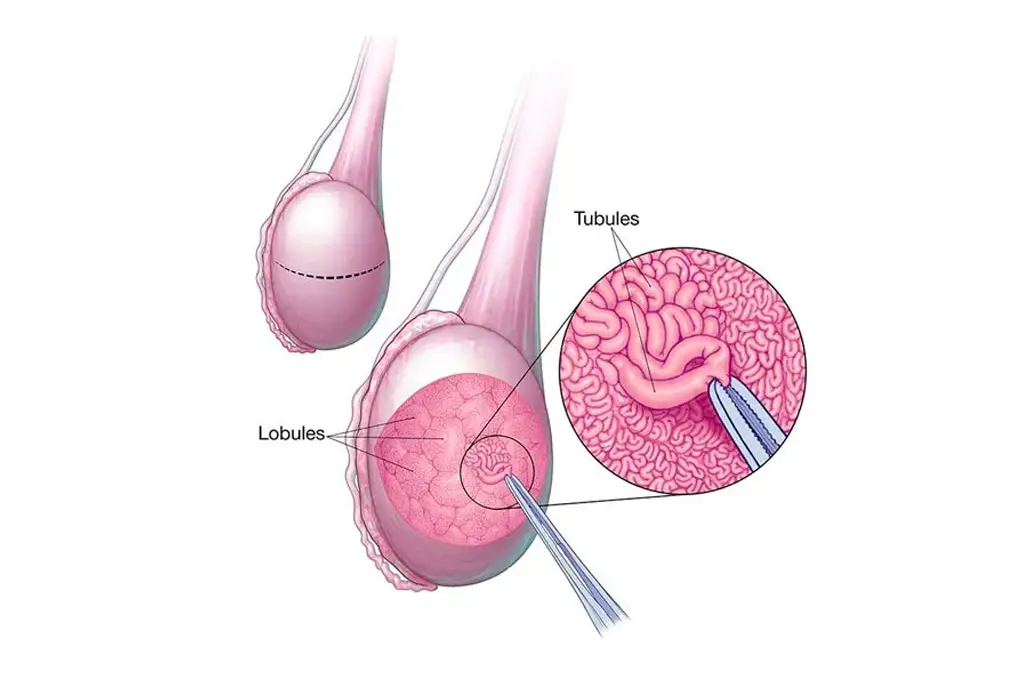
- While performing the microTESE procedure, the doctor will give you a general anaesthetic to help you sleep and be comfortable throughout the surgery. While you are sleeping, your surgeon makes a small incision (cut) in the centre of your scrotum. The surgeon will then uncover your testicles and examine them under a high-powered surgical microscope for enlarged seminiferous tubules (sperm-producing tubes). A bulging tube may contain sperm.
- Your surgeon will then extract tissue samples from the tubes in one testicle. Your surgeon will repeat this surgery on the other testicle. Finally, after extracting tissue samples from both tests, your surgeon will seal the wounds with very small stitches.
- The surgeon passes the tissue samples to an andrology doctor, and the doctor examines them under a microscope. The technologist spends time searching for sperm. If sperm is identified, the technician removes it and freezes it in liquid nitrogen. Then, you can use your frozen sperm for in vitro fertilisation (IVF). If sperm is present, you may notice it right away after surgery. Sometimes, you will receive an update the day after surgery.
What Is the Success Rate of MicroTESE Surgery?
The microTESE success rate is favourable for the majority of males. In fact, surgeons locate sperm in roughly 40-60% of microTESE treatments. If you intend to use all of your sperm for in vitro fertilisation (IVF), you may require more than one microTESE operation.
While microTESE is effective for many men, surgeons do not always detect sperm during the surgery. If this occurs and you decide to have microTESE again, your surgeon’s odds of successfully identifying sperm are extremely slim.
Are There Any Risks Related to MicroTESE Procedure?
MicroTESE is a minor surgical technique that has few potential risks. Most problems that emerge after MicroTESE can be managed conservatively. Here are some complications related to MicroTESE.
- There is a minor chance of bleeding and infection.
- The area may be painful for 2 or 3 days following surgery.
- The scrotum can become inflamed or discoloured. This normally resolves after a few days.
- You can have skin or testicular infections.
- There are also chances of testicle injury.
Conclusion
Note that sperm extraction via microTESE is only one step of the journey to parenthood. The sperm retrieved can be frozen and used for the IVF procedure. Suppose you have already consulted both a urologist and a reproductive endocrinologist before starting treatment. In that case, it is recommended that you discuss the whole process with them to arrive at the best treatment decision for your particular case. Microscopic Testicular Sperm Extraction (MicroTESE) offers a great means through which you and your partner can remain confident on your path to parenthood.