Recurrent Pregnancy Loss (RPL)
Recurrent Pregnancy Loss (RPL) is described as having two or more miscarriages. A complete physical examination is suggested after three repetitive miscarriages.
What is the probability of having repetitive miscarriages?
About 1% of females would experience repeated miscarriages.
What are the causes of RPL?
- Most miscarriages occur randomly when an unusual number of chromosomes reaches the embryo during fertilization.
- The biggest reason for RPL is an abnormal number of chromosomes in the embryo.
- Additionally, hormonal disorders (Diabetes and Thyroid problems), uterine problems, and immunological factors may also add to recurring miscarriages.
- Other reasons like smoking, caffeine and alcohol intake, exposure to toxic products, and being overweight may also add to the RPL.
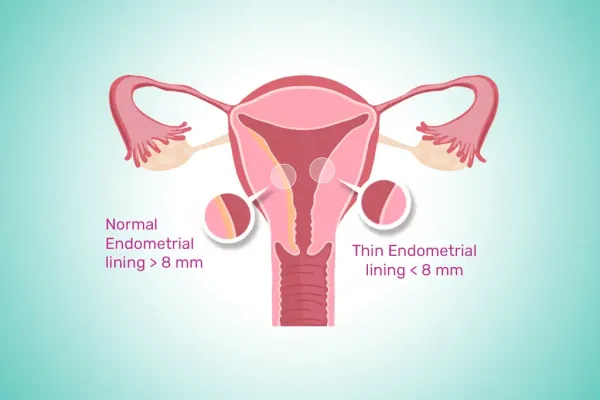
Uterine factors may involve:
- Inherited uterine deformities such as the uterine septum, double uterus.
- Presence of large polyps and submucosal fibroids
- Asherman’s syndrome (presence of scar tissue in the uterine cavity)
Genetic Factors (Aneuploidy)
Miscarriage results due to a chromosomal anomaly in the embryo.
In couples experiencing frequent miscarriages, one partner carries a chromosome in which a portion is relocated to another chromosome. The process is referred to as translocation. People with translocation typically do not present signs. Some chromosomal deformities can be seen in some of their eggs or sperm. If an embryo receives a high or low amount of genetic material, it may indicate a miscarriage.
Endocrine Disorders
Thyroid dysfunction and unregulated blood sugar levels is an indicator of RPL. Furthermore, owing to alterations in the endocrine profile, even PCOS patients carry a greater risk of pregnancy loss.
Is there any effect of other health conditions on the risk of miscarriages?
Females with health conditions are at an increased risk of frequent miscarriages.
- Antiphospholipid syndrome (APS) is an autoimmune disorder. In this, antibodies are formed by an individual’s immune system. These antibodies target certain substances that play a key role in blood clotting process. APS is found to be linked to RPL and fetal deaths.
- Females with a condition named PCOS or Polycystic Ovary Syndrome also carry a greater risk of miscarriage.
How is Recurrent Pregnancy Loss assessed?
- RPL can be assessed initially by taking the complete patient history and physical evaluation.
- A series of diagnostic tests can be done, including blood tests and uterus examination. This examination detects any deformities or acquired factors, including fibroids and polyps, that may hinder the embryo’s implantation.
- A genetic compatibility test can also be done on the couple to assess and predict the potential genetic deformity in the embryo.
How to treat Recurrent Pregnancy Loss RPL?
Treatment is recommended to women with recurrent pregnancy loss, depending on the underlying cause of it. The chance of a successful pregnancy is high. If a woman has experienced repeated miscarriages, it is important to consult with a doctor who can suggest appropriate treatments to reduce the risk of miscarriages.