What Are the Causes of Thin Endometrium?
The following are the thin endometrium causes:
- Hormonal imbalance: The lack of estrogen can be due to several things, such as stress, an unhealthy diet, and some medications.
- PCOS: It is the main cause, affecting 10% of reproductive-aged women.
- Age: This factor may also be an important factor because older women’s ovaries produce less amount of estrogen, and this leads to thin endometrium.
- Poor blood flow: The thickness of the endometrium is determined by the blood flow to the uterus. Insufficient blood flow to the uterus causes thinning. Poor blood flow can be due to smoking, obesity, high blood pressure, diabetes, and birth control pills.
- Damaged endometrial lining: Previous uterine infection can damage the lining and can cause scar tissue.
- Uterine fibroids: These are benign growths and can be so small that the human eye cannot detect them, or else these can be so large that they can cause bulges in the uterus. Fibroids can affect the chances of pregnancy; doctors may recommend surgery to remove this.
- Chronic endometritis: This refers to infection and or inflammation of the uterine lining, and it prevents the embryo from implanting.
- An abnormal menstrual cycle – seen mainly in hormonal disturbance and impaired ovulation may also be the main reason for the thin lining.
What Are the Symptoms of Thin Endometrium?
Following are the thin endometrium symptoms:
- Irregular or light periods: If periods become lighter or more irregular than usual, it can signify a thin endometrial lining.
- Infertility: Inability to achieve pregnancy.
- There is inadequate bleeding during menstrual periods.
- Many times, there may be no symptoms of the thin lining.
What Is Thin Endometrium Treatment?
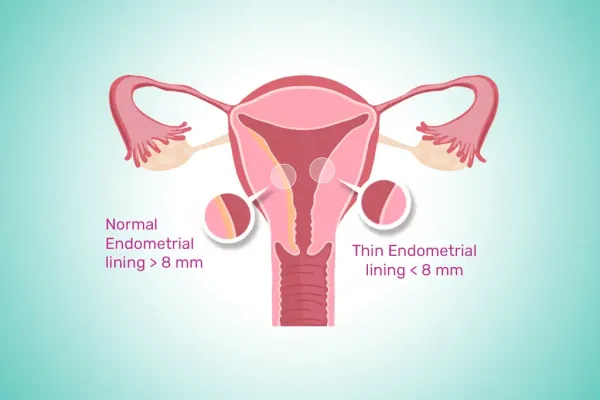
- The endometrium is the innermost layer of the uterus. An optimal endometrium is crucial for a regular menstrual cycle and successful pregnancy. The endometrium treatment involves finding the causative factor and treating that first.
- Hysteroscopy: This procedure helps a surgeon look inside the uterine cavity, and the surgeon evaluates the endometrial conditions. Intrauterine adhesions that cause thinning can be removed through this process. Signs of endometritis can be identified, and any polyps or small fibroids can be removed. A culture of endometrium and histopathological analysis will help find the pathogens causing this condition.
- Platelet-rich Plasma (PRP): This is a newer mode of treatment under review to help refractory patients of thin endometrium. PRP is an autologous blood plasma enriched with platelets 4-5 times above normal. It can stimulate proliferation and regeneration with many growth factors. PRP may aid in endometrial growth and its thickness.
- Estrogen therapy: Exogenous estrogen (the hormone that helps endometrial growth) may help promote endometrium, especially in perimenopausal women or in those with early menopause. This is available in tablets or transdermal local application forms.
Conclusion
Thin endometrium may lead to frequent miscarriages and infertility. We recommend a visit to a gynaecologist to seek the resolution of this problem. Avoidance of the symptoms may be problematic. With awareness and preventive care, thin endometrium won’t cause any major complications.